Atrial Rhythms
Premature Atrial Complexes (PAC's)
- Premature beats may be produced by the atria, AV junction, or the ventricles, and appear early (they occur before the next expected beat).
- PAC's occur when an irritable site within the atria discharges before the SA node impulse is due to discharge, thus interrupting the rhythm.
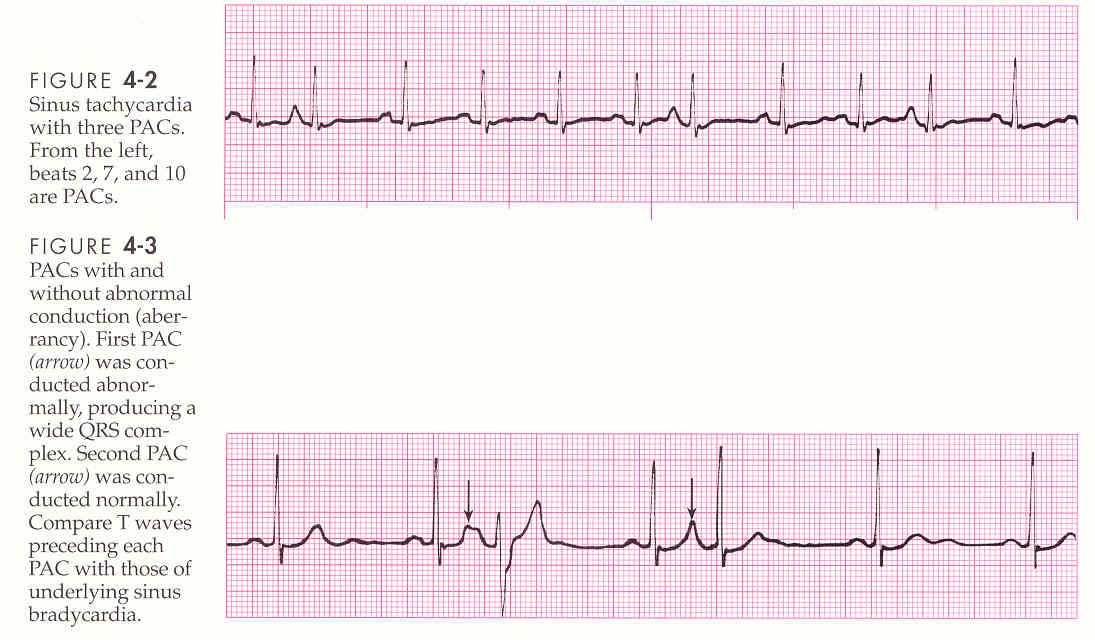
Characteristics of PAC's
- Rate is usually normal but depends on underlying rhythm.
- Rhythm is regular with premature beats.
- P waves are premature (occuring earlier than the next expected P wave), upright, one precedes each QRS complex, often differ in shape from sinus P waves (may be flattened, notched, pointed, biphasic), or lost in the preceding T wave.
- PRI may be normal or prolonged, depending on the prematurity of the beat.
- QRS is usually less than 0.10 seconds but may be wide, or absent, depending on the prematurity of the beat.
PAC Patterns
- Pairs (coupled): 2 sequential PAC's
- Runs or bursts: 3 or more sequential PAC's
- Atrial Bigeminy: Every other beat is a PAC.
- Atrial Trigeminy: Every thrid beat is a PAC.
- Atrial Quadrigeminy: Every fourth beat is a PAC.
Causes and Clinical Significance
- PAC's are common and may occur due to stress, CHF, MI, fatigue, digoxin toxicity, hypokalemia, hypomagnesemia, hyperthyroidism, excessive intake of caffeine, tobacco, or ETOH.
- Patient may c\o palpitations (if frequent) or may be unaware of the occurrence.
Interventions
- Usually none, if infrequent.
- Frequent PAC's may initiate episodes of a fib, a flutter, SVT, and are tx by correcting the underlying cause (decreased stress, decreased consumption of caffeine-containing beverages, tx CHF, correcting electrolyte imbalance). If needed, PAC's may be tx with beta-blockers, calcium channel blockers, or anti-anxiety meds.
Multifocal Atrial Tachycardia (MAT)
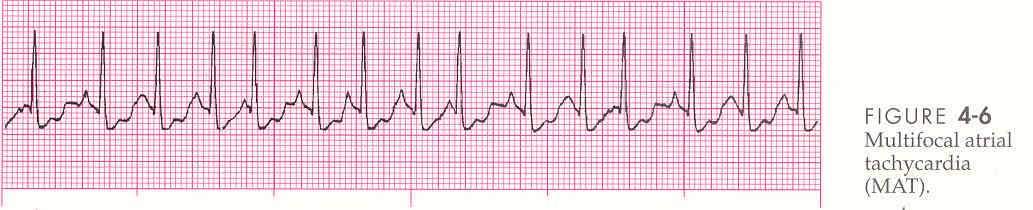
- When WAP is associated with a ventricular response of 100 bpm or greater.
- Multiple ectopic sites stimulate the atria.
- MAT is easily confused with afib because both rhythms are irregular, however, P waves (although varying in size, shape, and direction) are clearly visible in MAT.
Causes and clinical Significance
- MAT is most commonly observed in the elderly and in people with severe chronic COPD, MI, hypoxia, and electrolyte imbalances.
Interventions
- Tx is directed at the underlying cause.
- If the patient is stable but symptomatic, and has normal cardiac fx, meds may include beta-blockers, calcium channel blockers, or amiodarone.
- Tx of stable but symptomatic patients with impaired cardiac fx includes amiodarone or diltiazem.
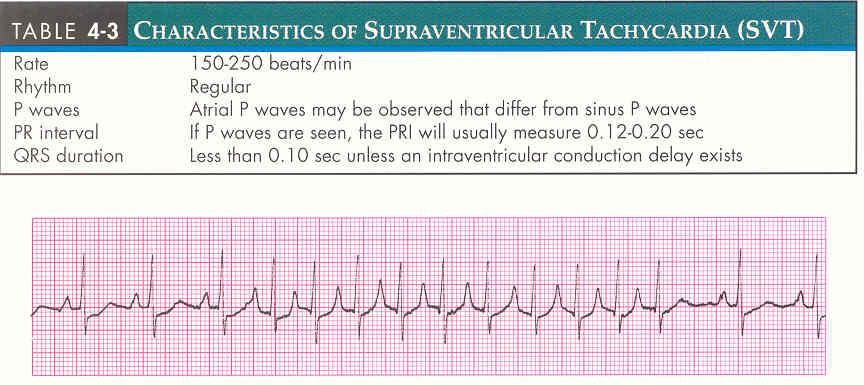
Supraventricular Tachycardia (SVT)
- Refers to a rhythm with a rapid ventricular rate and a narrow QRS complex, but whose specific origin (atrial or junctional) is uncertain.
- An SVT that suddenly starts or ends is called Paroxysmal Supraventricular Tachycardia (PSVT).
Characteristics of SVT
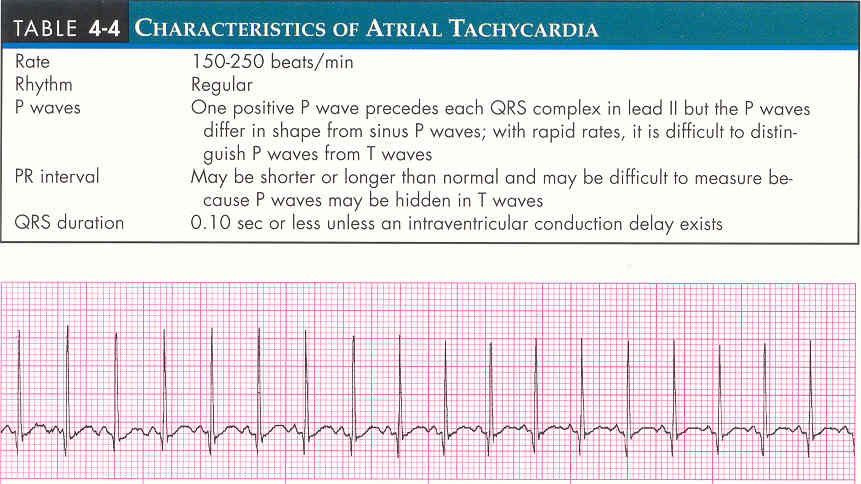
Atrial Tachycardia
- 3 or more sequential PAC's occurring at a rate of greater than 100 bpm.
- Atrial tachycardia that starts or ends suddenly is called Paroxysmal Atrial Tachycardia (PAT). PAT may last for minutes, hours, or days.
- Atrial tachycardia is a series of rapid beats from an atrial ectopic focus, often precipitated by a PAC. The rapid rate overrides the SA node and becomes the pacemaker.
- Conduction of the atrial impulse is frequently 1:1 (every atrial impulse is conducted to the ventricles).
- Carotid sinus pressure will either abruptly end/convert the dysrhy to a sinus rhythm or have no effect at all.
Characteristics of Atrial Tachycardia
Atrial Flutter
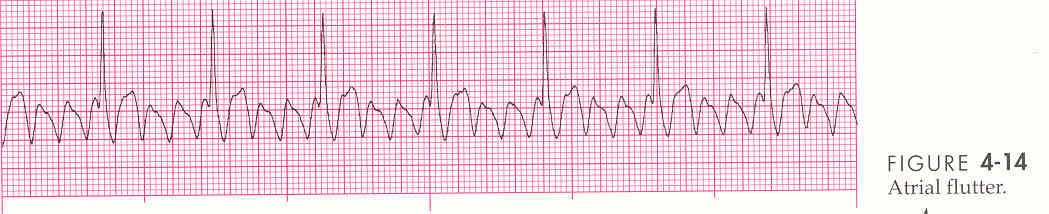
- An irritable site depolarizes regularly at an extremely rapid rate.
- An irritable focus within the atrium typically depolarizes at a rate of 300bpm. If each impulse was transmitted to the ventricles, the ventricular rate would equal 300 bpm. The healthy AV node protects the ventricles from these extremely fast atrial rates.
- Normally, the AV node cannot conduct faster than approx. 180 bpm. Thus, at an atrial rate
of 300 bpm, q other impulse arrives at the AV node while it is still refractory -
(the state in which a cell is able to respond to a stimulus).
- The resulting ventricular response of 150 bpm is called 2:1 conduction. The ration of the atrial rate (300 bpm) to the ventricular rate (150 bpm) is 2-to-1.
- Conduction ratios are usually even (2:1, 4:1, 6:1).
Characteristics of Atrial Flutter
- Rate - Atrial rate is 250-450 bpm (typically 300 bpm). Ventricular rate is variable but usually does not exceed 180 bpm.
- Rhythm - Atrial is regular. Ventricular is regular or irregular.
- P waves - none identifiable. Saw-tooth "flutter" waves are present.
- PRI is not measurable.
- QRS is usually less than 0.10 seconds but may be widened if flutter waves are buried in the QRS complex.
Causes and Clinical Significance
- Atrial flutter is usually precipitated by a PAC.
- Chronic atrial flutter is unusual because the rhythm usually reverts to sinus rhythm or A-fib, either spontaneously or with tx.
- Atrial flutters may occur in conditions such as: PE, ETOH intoxication, hypoxia, ischemic heart ds, or digoxin toxicity.
- Most often occurs in patients with mitral or tricuspid valve ds, but may rarely occur in patients without cardiac ds.
- Severity of s/s vary. The more rapid the ventricular rate, the more likely the patient is to be symptomatic. Patient may experience palpitations, skipped beats, weakness, dizziness, or CP.
Interventions
- When A-flutter is present with a 2:1 conduction, it may be difficult to differentiate the dysrhythmia from ST, PSVT, etc. Vagal maneuvers may temporarily slow the AV conduction and reveal the underlying flutter waves.
- In cases with A-flutter associated with a rapid ventricular rate, tx is first directed at controlling the ventricular response with calcium channel blockers (verapamil, diltiazem) or beta-blockers (metoprolol, propranolol) if cardiac function is normal.
- If cardiac fx is impaired, meds such as digoxin, diltiazem, or amiodarone may be used.
- If patient exhibits serious s/s (SOB, CP, hypotension, decreased LOC, acute MI, CHF) due to rapid ventricular rate, cardioversion may be performed.
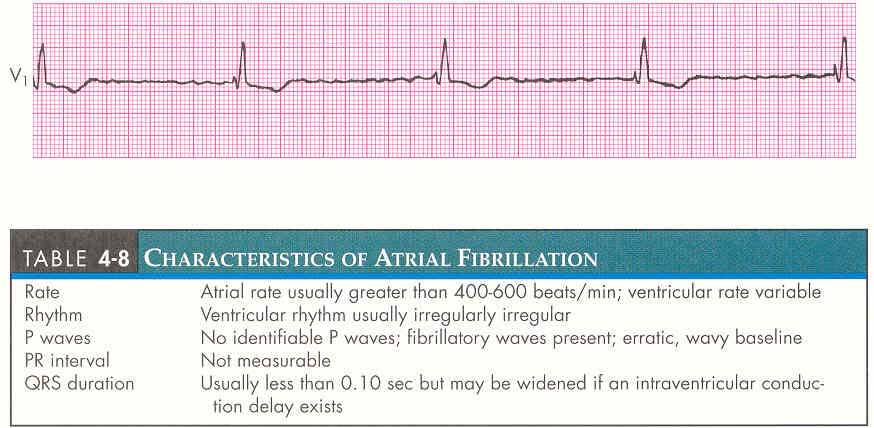
Atrial Fibrillation (AFIB)
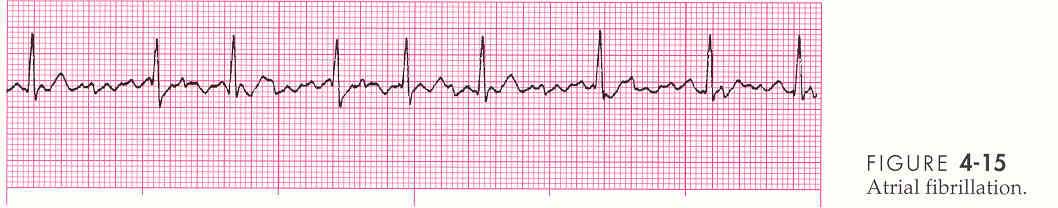
- This dysrhythmia may occur acutely (less than 48°), paroxysmally (intermittent), or chronically (greater than 1 month).
- In AFIB, the atria are depolarized at a rate of 400-800 bpm.
- The rapid impulses causes the atrial muscles to quiver (fibrillate), resulting in ineffective atrial contraction, a subsequent decrease in C.O., and a loss of atrial kick.
Characteristics of AFIB
Causes and Clinical Significance
- Conditions commonly associated with AFIB are rheumatic heart ds, CAD, HTN, CHF, PE, hypoxia, cardiomyopathy, pericarditis, drugs, or intoxicants (ETOH, carbon monoxide), acute/chronic pulmonary disease, enhanced vagal tone, hypokalemia, hyperthyroidism.
- Paroxysmal AFIB has been associated with excessive ETOH consumption in otherwise healthy individuals "holiday heart syndrome."
- Patients experiencing AFIB may develop intra-atrial emboli because the atria are not contracting, and blood stagnates in the atrial chambers. This predisposes the patient to systemic emboli, particularly stroke, if the clots dislodge spontaneously or because of conversion to a sinus rhythm.
- Severity of s/s varies. The more rapid the ventricular rate, the more likely the patient is to be symptomatic.
- AFIB with a rapid ventricular response may produce s/s such as lightheadedness, palpitations, dyspnea, CP, and hypotension.
Interventions
- In the stable patient with AFIB associated with a rapid ventricular response, tx is
first directed toward controlling the ventricular response, rather than converting the
dysrhythmia to a sinus rhythm.
- If cardiac fx is normal, calcium channel blockers ir beta blockers may be used.
- If cardiac fx is impaired, meds such as digoxin, diltiazem, or amiodarone may be used.
- To convert AFIB to sinus rhythm, procainamide, or antidysrhythmics (amiodarone) may be used.
- If patient exhibits serious s/s (SOB, CP, hypotension, decreaseed LOC, acute MI, CHF) because of rapid ventricular rate, cardioversion may be considered.
- Elective cardioversion may be performed in patients that fail to respond to an initial trial of meds. Anticoagulation is recommended for any patient undergoing elective cardioversion. Usually, it is used prophylactically 2-3 weeks prior to cardioversion and continues for about 4 weeks afterwards.
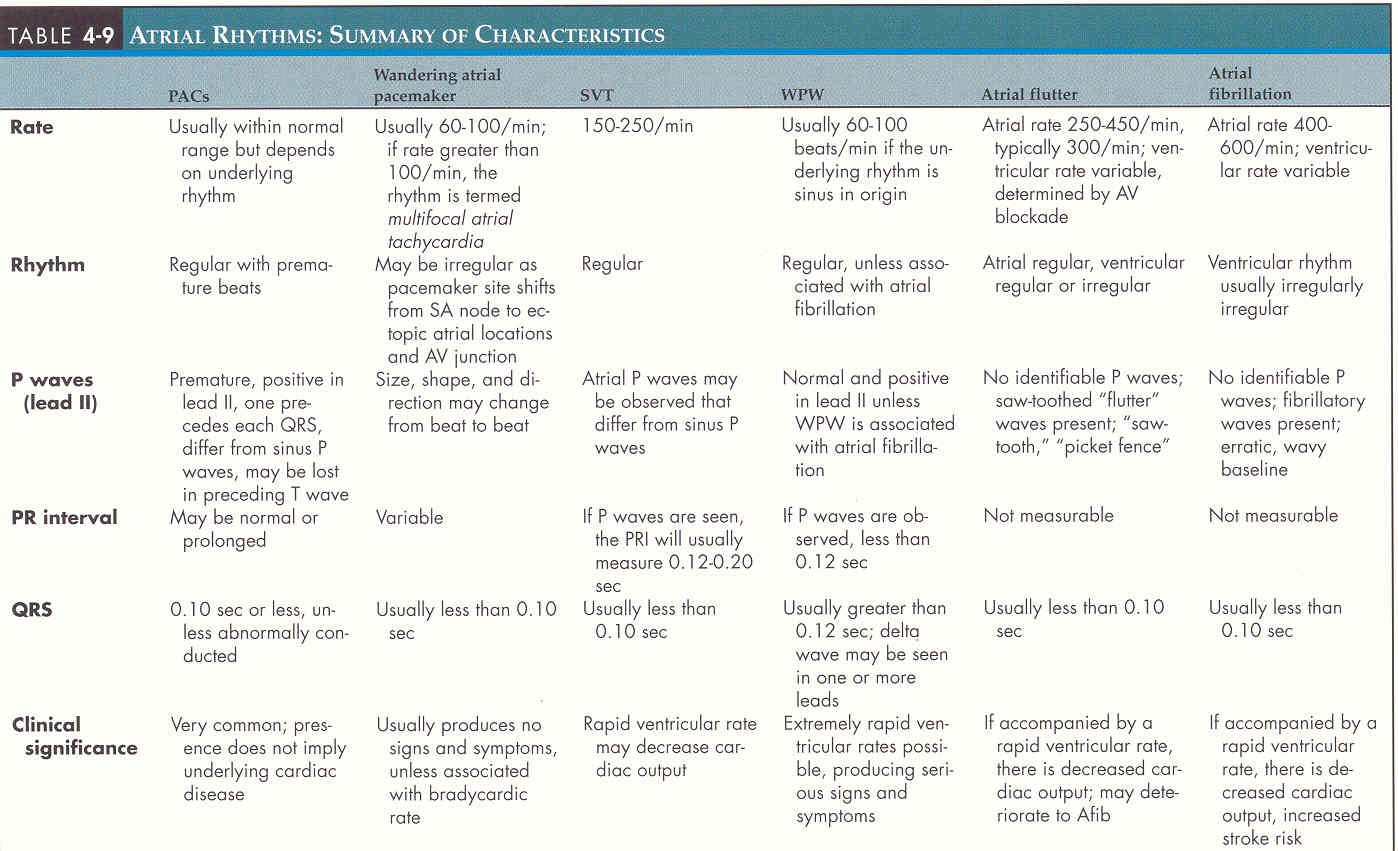
Summary of Characteristics
↑ Top of Page ↑