Atrioventricular Blocks
First Degree AV Block
- In 1° HB, impulses from the SA node to the ventricles are delayed (not blocked).
- 1° HB usually occurs at the AV node.
- In 1° HB, all components of the ECG tracing are usually within normal limits except the PRI. This is because electrical impulses flow normally from the SA node through the atria, but there is a delay in conduction.
- Despite its name, in 1° HB, impulses are delayed, not blocked.
- All sinus beats are conducted.
- Impulses are delayed for the same period before they are conducted to the ventricles. This delay in AV conduction results in a PRI greater than 0.20 seconds in duration and constant.
Characteristics of 1° HB

Causes and Clinical Significance
- 1° HB may be a normal finding in individuals with no history of cardiac ds, especially in athletes.
- 1° HB may also occur because of ischemia or injury to the AV node or junction, med therapy (quinidine, procainamide, beta blockers, calcium channel blockers, digoxin, and amiodarone), rheumatic heart ds, hyperkalemia, acute MI, or increased vagal tone.
- Approximately 5-10% of patients with acute MI have 1° HB at some point during the peri-infarct period.
Interventions
- Often asymptomatic; however, marked 1° HB can lead to symptoms even in the absence of higher degrees of AV block.
- 1° HB that occurs with acute MI should be monitored closely.
Second Degree AV Blocks
- An intermittent disturbance in conduction of impulses between the atria and ventricles.
- Some, but not all, atria impulses are blocked from reaching the ventricles.
- Because the SA node is generating impulses in a normal manner, each P wave will occur at a regular interval across the rhythm strip (all P waves will plot through on time), although not every P wave will be followed by a QRS complex. This suggests that the atria are being depolarized normally, but not every impulse is being conducted to the ventricles. As a result, more P wave than QRS complexes are visible.
- 2° HB is classified as type I or II, depending on the location of the block above (type I) or below (type II) the bundle of His.
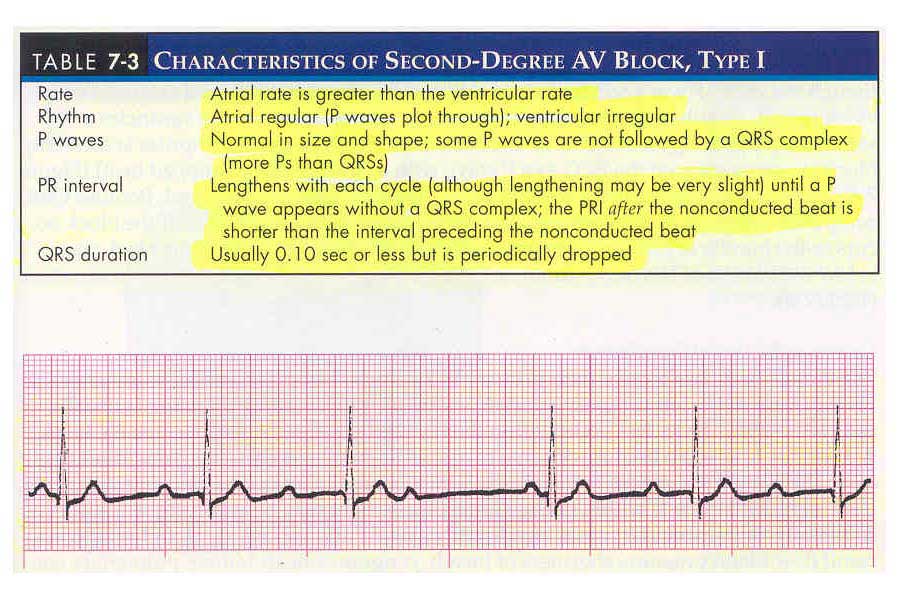
2° HB Type I (Wenckebach, Mobitz Type I)
- The conduction delay usually occurs at the level of the AV node.
- Impulses generated by the SA node take longer and longer to conduct through the AV node, appearing on the ECG as lengthening PRI's. The lengthening PRI's eventually result in a P wave that falls during the refractory period of the ventricles. Because the ventricles are refractory, the sinus impulse is blocked, which appears on the ECG as a P wave with no QRS complex after it (dropped beat).
- The atria are depolarized (represented by the P wave), but the AV junction fails to conduct the impulse from the atria to the ventricles (reflected as the absence of a QRS complex).
- Because the QRS complexes are periodically dropped, the ventricular rhythm is irregular.
Characteristics of 2° HB Type I
Causes and Clinical Significance
- Commonly associated with AV nodal ischemia 2° to occlusion of the right coronary artery.
- Occurs because of increased parasympathetic tone or the effects of meds (digoxin, beta-blockers, verapamil).
- When associated with acute inferior wall MI, the dysrhythmia is usually transient, resolving within 48-72 hours.
- 2° HB type I may progress to 3° HB (complete block).
Interventions
- Usually asymptomatic because the ventricular rate often remains nearly normal and C.O. is not significantly affected.
- If patient is symptomatic and the dysrhythmia is a result of meds, these substances should be withheld.
- If heart rate is slow and serios s/s (decrease BP, SOB, CHF, PE, decreased LOC, pulmonmary congestion) occur due to decreased heart rate, atropine and/or temporary pacing should be considered.
- When this dysrhythmia occurs in conjunction with acute MI, the patient should be observed for increased HB.
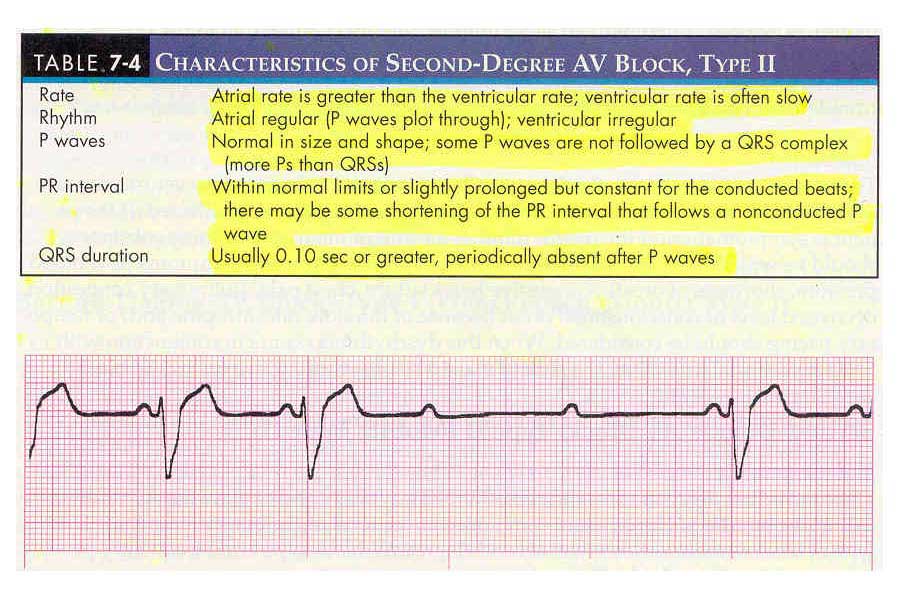
2° Type II (Mobitz, Type II)
- Conduction occurs below the AV node, either at the bundle of His, or more commonly, the bundle branches.
- More serious than 2° HB type I and frequently progresses to 3° HB (complete block).
- Because the SA node is generating impulses at a normal manner, each P wave occurs at a regular interval across the rhythm strip (all P waves will plot through on time), although not every P wave will be followed by a QRS complex.
- Impulses generated by the SA node are conducted to the ventricles at the same rate (appearing as a constant PRI) until an impulse is suddenly blocked, appearing as a P wave with no QRS after it (dropped beat).
- Because QRS complexes are periodically dropped, the ventricular rhythm is irregular.
- If the block occurs in the bundle of His (uncommon), the QRS will remain narrow. If the block occurs below the bundle of His (more common), the QRS will be greater than 0.10 seconds in duration.
Characteristics of 2° HB type II
Causes and Clinical Significance
- The bundle branches receive their primary blood supply from the left coronary artery. Thus, ds of the left coronary artery or an anterior MI is usually associated with blocks that occur within the bundle branches.
- 2° HB Type II may also occur because of acute myocarditis, or other types of organic heart ds.
- If the ventricular rhythm is within normal limits, the patient may be asymptomatic. More commonly, the ventricular rate is significantly slowed and s/s result (decreased BP, SOB, CHF, decreased LOC, pulmonary congestion) because of the slowed heart rate and C.O.
- Patients with 2° HB Type II are often symptomatic, have a compromised prognosis, and commony progress to 3°.
Interventions
- If symptomatic, TCP should be instituted until a PPM can be inserted.
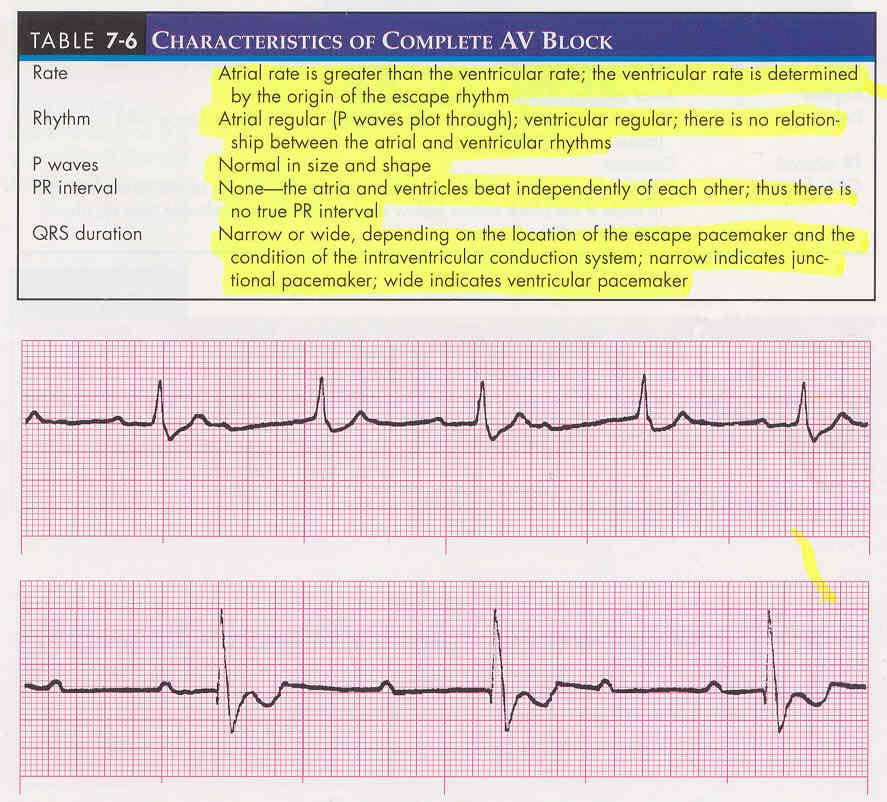
Complete AV Block (3° HB)
- The atria and ventricles beat independently of each other.
- Impulses generated by the SA node are blocked before reaching the ventricles.
- Block may occur at the AV node, bundle of His, or bundle branches.
- A secondary pacemaker (either junctional or ventricular) stimulates the ventricles; therefore, the QRS may be narrow or wide, depending on the location of the escape pacemaker.
- 3° HB associated with an anterior MI is usually preceded by 2° HB Type II.
Characteristics of 3° HB
Causes and Clinical Significance
- 3° HB has an incidence of 5.8% in the early period of acute MI and is nearly twice as common with inferior/posterior infarctions compares with anterior MI.
- When associated with an inferior MI, 3° HB often resolves on its own (within a week).
- 3° HB associated with an anterior MI may develop suddenly and without warning, usually 12-24 hours after the onset of acute ischemia.
- 3° HB with narrow QRS complexes is more stable than 3° HB with wide QRS complexes.
Interventions
- S/s will depend on the origin of the escape pacemaker and the patient's response to a slower ventricular rate.
- If QRS is narrow and the patient is symptomatic, initial management consists of atropine and/or TCP.
- If QRS is wide and the patient is symptomatic, TCP should be instituted while preparations are made for insertion of a PPM.
Summary of Characteristics

↑ Top of Page ↑